Popular heartburn drugs found to promote deadly superbug infections
04/05/2017 / By Russel Davis
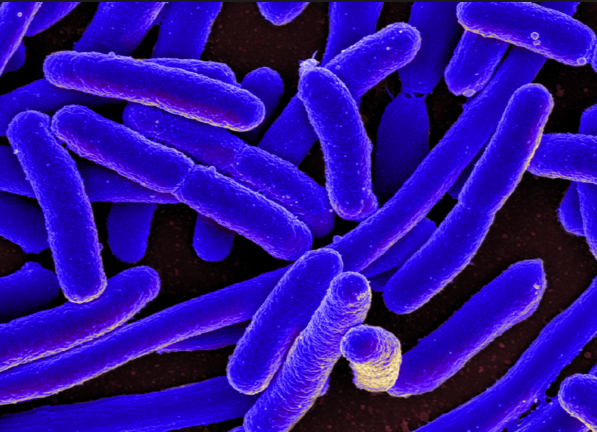
Acid reflux drugs raise the odds of Clostridium difficile infections, according to an analysis published in The Journal of the American Medical Association Internal Medicine. C. difficile is a bacterium that causes a condition called colitis, which is characterized by inflammation of the colon. Symptoms of colitis include fever, diarrhea and abdominal pain, as well nausea and loss of appetite.
Researchers examined 16 various studies comprised of a total of 7,703 patients with with C.difficile. The analysis showed that more than 50 percent of patients were using acid reflux medications. Data also showed that 20 percent of all patients developed recurrent C. difficile within three months of a previous infection. Of these patients, more than 22 percent were taking acid reflux drugs, compared with 17.3 percent of patients not taking the heartburn medications.
According to Dr. Sahil Khanna, one of the study’s lead researchers, suppressing stomach acid through heartburn medications has an effect on the bacteria living in the gut, which in turn increases the likelihood of C.difficile infection in patients. People taking the acid reflux drugs may already have worse health than their non-medicated peers at the onset of the study, which renders them highly-susceptible to infections.
“Patients with C.difficile should be reevaluated to assess the necessity of using gastric acid suppression medications,” said Dr. Khanna, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota.
However, an outside expert said the findings should not cause alarm among patients and clinicians.
“We don’t see this as a problem, because so many people are on these drugs. I wouldn’t change anything in what we do medically or tell patients based on what this meta-analysis found,” Dr. David Bernstein said. Dr. Bernstein is the Chief of Hepatology at Northwell Health in Manhasset, New York.
GERD drugs tied to C.diff infection in previous studies
Numerous studies have already identified a correlation between acid reflux medications and the onset of C. difficile infection. A 2016 study published in the journal Gut and Liver found that proton pump inhibitors were associated with C. difficile infection in critically ill patients. Researchers examined more than 1,000 patients who were admitted to intensive care units between August 2005 and July 2012. Study data showed that 6.7 percent of patients using PPI medications developed C. difficile infection, compared with only 1.8 of patients who took H2-blockers.
Another study has linked proton pump inhibitors to the onset of C. difficile infection in patients. Dutch researchers assessed the gut bacteria composition of more than 1,800 adults and found that PPI users exhibited less diversity in the gut microbiome. PPI users also displayed higher levels of bacteria commonly found in the mouth. Researchers said proton pump inhibitors reduce the stomach’s acidity, which in turn helps more oral bacteria to survive in the gut. The findings were published in the journal Gut.
In addition, a study published in the journal Clinical Infectious Diseases revealed that acid reflux drugs may raise the odds of infection-related mortality in users. An analysis of 485 patients with C. difficile infections showed that 19 of 23 patients who died of the infection took prescription acid suppressants 90 days prior to their hospitalization. The medications were also associated with a host of complications that cause ICU admission, surgery, or an abnormally dilated colon, researchers noted.
In 2012, the U.S. Food and Drug Administration has issued a warning on using acid reflux medications, stating that popular proton pump inhibitors — such as Nexium, Prilosec, and Prevacid — may raise the odds of contracting C. difficile infection. The agency advised health care professionals to consider a diagnosis of C. difficile-related diarrhea if PPI-medicated patients exhibit diarrhea that was not improving. The FDA has also urged patients to take the lowest possible dose for PPI.
Sources:
Tagged Under: acid reflux, C. difficile, Gastrointestinal system, GERD